The inappropriate use of antibiotics in clinical settings is a major driver of antibiotic resistance. A report by the UK Health Security Agency (UKHSA) found that at least 20% of all antibiotics prescribed in primary care in England were inappropriate.
One way to overcome this challenge is by developing effective diagnostic tests. A diagnostic test could support a physician’s decision not to use antibiotics, for example by ruling out bacterial infection or conforming viral infection, thereby minimising the unnecessary use of antibiotics and promoting use of the most appropriate (targeted) antibiotic to treat an infection.
Currently, many hospitals around the world rely on traditional culture-based methods to identify bacterial infections and conduct antibiotic susceptibility testing. This requires bacteria from patient samples to be grown, or cultured —a process that can take 2 to 3 days.
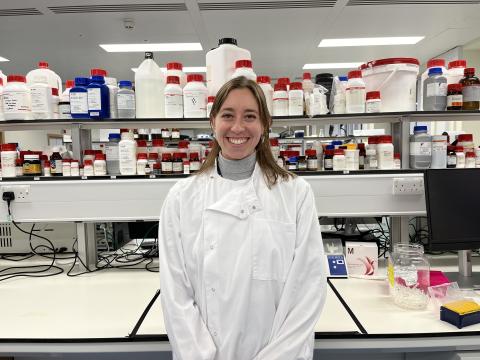
To overcome this challenge, Dr Sara Keller, Postdoctoral Research Assistant in Oxford's Department of Engineering Science is developing ultrasound molecular imaging probes to rapidly and specifically diagnose bacterial infections. The aim is to create new tools for image-guided interventions, to mitigate unnecessary antibiotic prescriptions. Diagnostics are proven to enhance the appropriate use of antibiotics, which will reduce the burden of antibiotic resistant infections.
Based at Oxford’s Biomedical Ultrasonics, Biotherapy, and Biopharmaceuticals Laboratory (BUBBL), Sara’s research involves microbubbles, gas-filled spheres traditionally used as imaging agents.
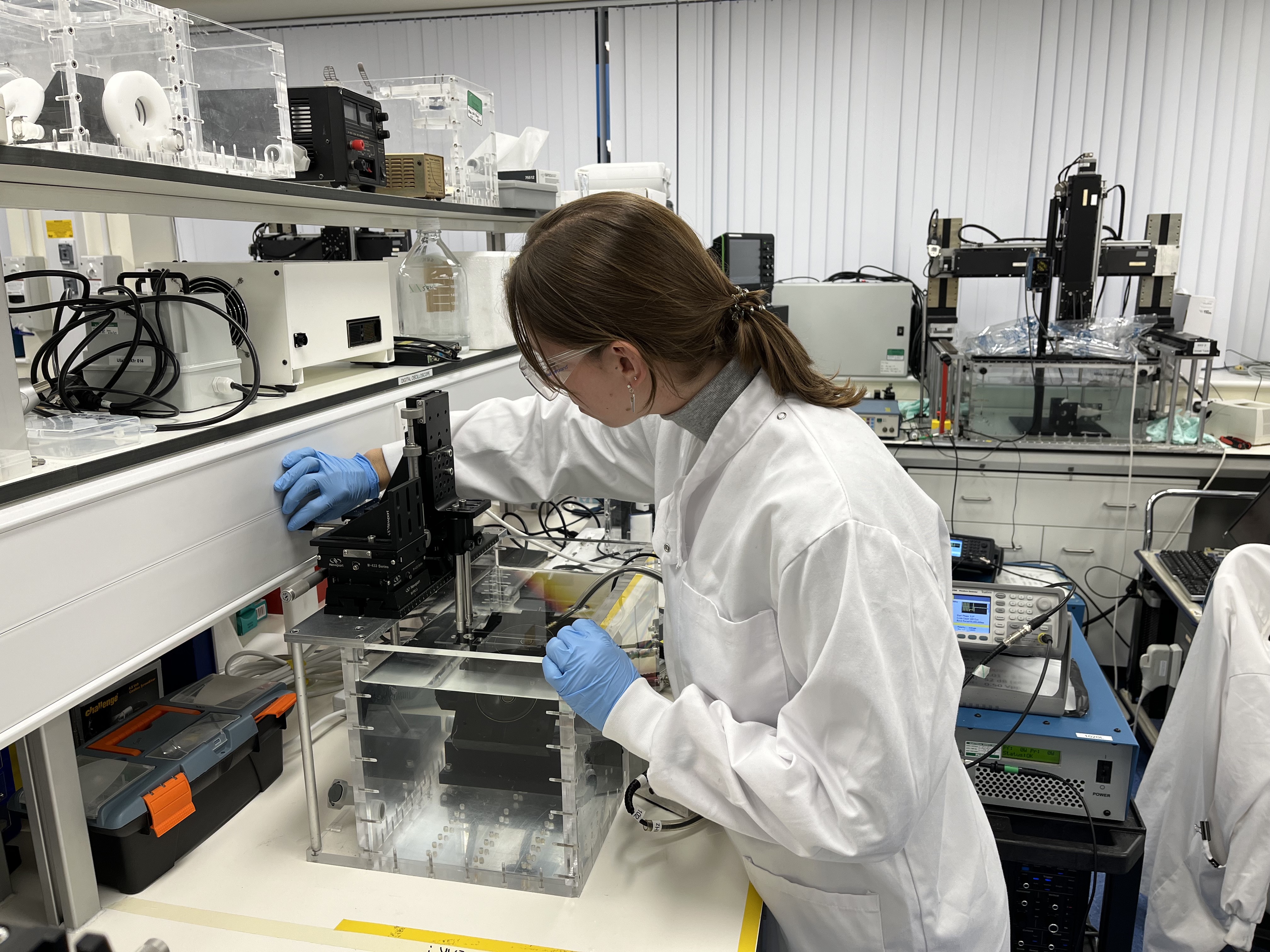
Microbubbles are made of a lipid shell surrounding an inert gas and are easily modified with ligands to increase their specificity to a target in vivo, in the patient’s body. Adding targeting agents can enable real-time molecular imaging of infections and reduce the waiting time associated with culture-based methods. This method is also minimally invasive, requiring delivery of contrast agents to the site of infection via an injection or intravenously.
Sara is currently working on the formulation and development of physiologically relevant in vitro biofilm models, with the aim to expand into more complex models in the future. She is also investigating the “theranostic” potential, meaning a combination of therapeutic and diagnostics, of these imaging agents to allow for image-guided biofilm removal.
On next research steps, Sara said, “In BUBBL, we care a lot about the translation of new technologies to benefit patients. To facilitate this application, we will now look to seek clinician and patient input on how to effectively move these exciting research developments into clinical practice to tackle AMR. The Beyond Antibiotics team have built relationships with plastic and orthopaedic surgeons, guiding our focus on the diagnosis and treatment of biofilm-associated infections within chronic wounds and implants.”
AMR is an incredibly complex and challenging problem, which is part of what makes it such an interesting research area to work in. I believe it is going to take huge interdisciplinary effort to develop solutions that help patients and I’m very glad to play a role in that.